Stewart is a locum operating department practitioner currently working at University Hospitals Coventry and Warwickshire NHS Trust

Up until four weeks ago I was based in a private hospital in Lincolnshire, employed by an agency that supplied locum professionals to private hospitals. Prior to this I trained to become an ODP with the NHS before moving into agency work as scrubs for orthopaedics. I had been doing this for close to 20 years, but my contract with the agency came to an abrupt end as soon the COVID-19 crisis hit.
When the pandemic began to ramp up, the private sector started to close down for several agency and locum workers across the nation. I, however, found myself in a fortunate situation. I was in the process of transitioning to a new contract with an agency that supplied locum staff to NHS hospitals. I had wanted for some time to get back into the NHS to further my experience and gain new skills for CPD.
I was due to work in emergency general surgery but the pressures of COVID-19 had started to intensify at this point and was asked almost immediately if I wouldn’t mind supporting the ITU and emergency theatres in the hospital. I absolutely wanted to work and support in whichever way I could.
I was quickly placed on training sessions provided by the hospital. This included full PPE donning and doffing taught and demonstrated by an anaesthetist. We practiced this in safe environments, so we could get used to the protective wear and how it feels. It is hot and sweaty and also challenging to have three pairs of gloves on but as an ODP I am used to working in long periods in gowns and scrubs for orthopaedics.
I took part in fit testing for the tight-fitting respirators. In this training, you are first asked to breathe normally inside a clear plastic helmet, an onion smelling substance is squeezed through a hole in the helmet and you are asked if you can taste or smell the substance. If you can’t taste anything then you will immediately fail that part, but luckily I passed. The next thing is to try the FFP3 mask, these masks in particular rely on having a good seal with your face. The face fit test is carried out to ensure the respiratory protective equipment can safely protect the wearer. The idea is that you are not supposed to taste or smell the substance anymore as the seal should fit perfectly around your face. Once I passed this, I was good to go.

When I was moving from a private background to the NHS, I presumed that there will be differences in culture, but the atmosphere was charged. Colleagues have been supportive and there is a real sense of bonding that goes on in the theatre. Colleagues care for each other. We share a common experience daily, because we are all in a dangerous situation together. You cannot social distance in an operating department - it is impossible - but it is a safe environment and everything needs to be kept clean.
It has been very hard for colleagues who are isolating from their families in order take care of patients. I have also not been able to spend time with my 15 year-old daughter, but have had the opportunity to wave at her from a distance through a window.
My most humbling experience has been working in the COVID-19 positive ITU unit. In my second week I found myself on the anaesthetic emergency response team face to face with my first awake COVID-19 patient. As I said hello to the middle-gentleman, I realised that we were in a real battle not just for patients, family and loved ones, but for people everywhere. It hit me that life will never be the same again.
I have seen people in their 40s and younger fighting for their lives on ventilators. The saddest part is when you see an empty bed a few days later and you know it is because that person sadly didn’t make it.
I have a complete and utter respect for the staff who are PPE-ed up for 13 hours. It is so tough. You try and do your best for people. Patients are very well looked after and we do our best to provide them with best care possible.
How do I feel? Scared at times. Seeing patients fight for their lives can be challenging but you still go in to work and do what you can.
My love for the human race keeps me going. I am grateful for members of the public, they have been wonderful. We have received food packages, drinks and toiletries. We also received lots of adorable rainbow pictures from children. The love and appreciation from the public has been incredible.
I have booked myself in for mental health counselling. This is something I have chosen to do now rather than waiting for symptoms of PTSD associated with working in a high stress environment. I feel it is important to prepare myself in case I suffer in the long term. The hospital also have wonderful facilities. As an agency locum professional, I may not have access to some of these, so I have booked my counselling privately.
I know that lack of access to support is one reason why other locums have not joined the NHS. Fully employed NHS staff will have access to cover in the event of falling sick, but agency workers don’t have this protection only universal credit. It has raised questions amongst locums, such as how are we covered if we put ourselves out in danger? What would happen to our families in the event that you contracted COVID-19? There needs to be a gentle reminder that we are vital healthcare workers too.

It is a surreal and daunting time for ODPs and other HCPC registered professionals, but it is a wonderful opportunity to make a difference and save lives. It is a real sacrifice, but I would encourage professionals with the skills to get involved where they can. You will feel a sense of pride knowing you are protecting lives in one way or another.
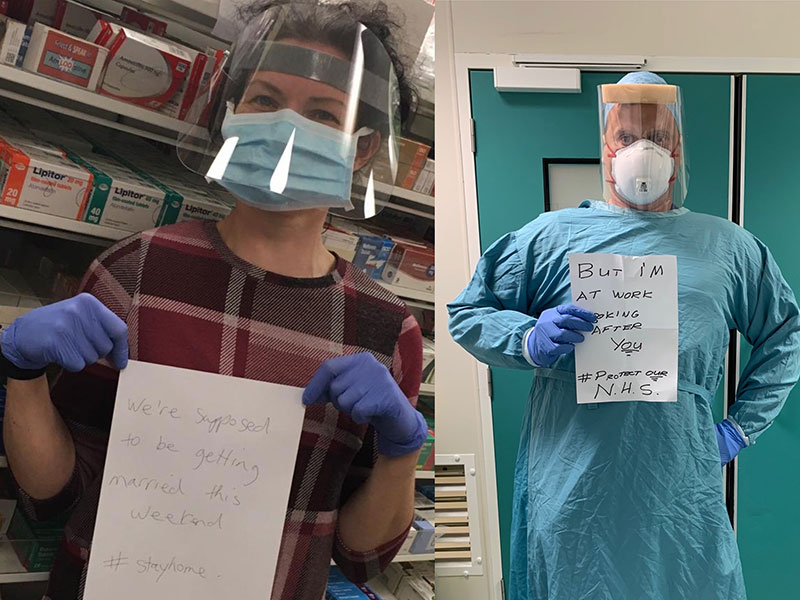
Here are a couple of images of me and my bride to be Clare, we were due to get married on 18 April 2020 at Eaglesfield in Scotland.
#StayHome #StaySafe.

- Published:
- 24/04/2020
- Resources
- In your words
- Subcategory:
- COVID-19
- Audience
- Registrants
- Profession
- Operating department practitioners

